
Germany-based neurosurgeon Professor Veerle Visser‐Vandewalle shares her experience of the latest DBS technology from Boston Scientific, how it’s helping her to personalise treatment for people with Parkinson’s – and why she believes in supporting patients “as a whole”
Professor Veerle Visser‐Vandewalle has focused on Deep Brain Stimulation as a Parkinson’s disease treatment for the last 24 years. As head of stereotactic and functional neurosurgery at the University Hospital in Cologne, Germany, she is a firm believer in the technology’s potential to improve the quality of life for many with the condition, by treating both motor and non-motor symptoms.
Deep Brain Stimulation (DBS) works by sending electronic signals through thin wires to specific parts of the brain that control movement. “We’ve seen that this has a positive effect on, for example, sleep disturbances and autonomic dysfunction in Parkinson’s patients,” she explains.
While DBS has been available as a treatment for decades, Professor Visser‐Vandewalle believes that the advent of new technology can make it even more effective and easy to use. But, as every person with Parkinson’s disease is different, finding a system that can be adapted to fit the needs of individual patients is crucial.

“It’s important we not only focus on the movement disorder itself, but we also look to the patients as a whole,” she says, pointing out that Parkinson’s can come with a range of complex challenges, including symptoms like depression and anxiety.
To address some of these challenges she has decided to use the Vercise Genus™ system from Boston Scientific, which allows her to control stimulation precisely whilst minimising side effects.
“Patients actually can forget that they are using DBS,” she says of the unit’s size, “and they are not confronted with a big pulse generator that continuously reminds them that they are using the treatment.” In fact, she adds, the extension cable is so thin that it can barely be seen in the neck of the patient.
Its design also means that many people might find it more comfortable: “Only one cable is needed for a patient implanted with two electrodes,” she explains, “so it may reduce the pulling sensation that some people may feel, due to the formation of scar tissue around cables.”
A comfortable advantage
The device also gives people the choice of a rechargeable or battery. Professor Visser‐Vandewalle explains that some don’t mind recharging their stimulator once a week if it means their battery will last 25 years – while others may decide they want to forget about the battery for a few years until it needs replacing.
Another benefit is that users of the system can, under certain conditions, undergo an MRI scan with the device attached, she says.
The device’s Bluetooth technology, which allows it to be programmed from three metres away, has been a useful feature recently – allowing for social distancing between healthcare professionals and people with Parkinson’s during the COVID-19 pandemic. It also means that a medical team can adjust the stimulation when a patient is walking and understand the direct effect this has on their gait.
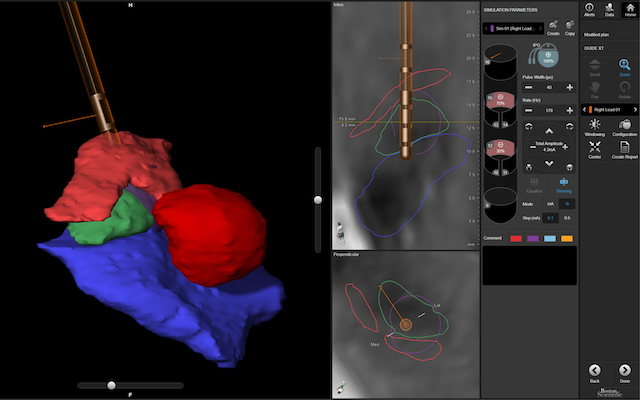
Clinicians can also use a compatible visualisation software called Guide-XT, which shows patient-specific anatomy with a 3D-visualisation, to plan the programming of the DBS device and understand stimulation field models within the brain.
All this helps to ensure that treatment can be tailored to specific patients’ symptoms. This adaptable approach is the perfect fit for Professor Visser‐Vandewalle’s priorities as a neurosurgeon: “My goal is to offer the patient an individualised treatment that reduces symptoms without side effects or any other burden.”
New technologies to treat Parkinson’s are emerging and improving. But while DBS has long been available to people who do not respond to certain medications, Professor Visser‐Vandewalle says that it is still relatively little-known, even among those with the condition.
“It is still a challenge to reach all patients to inform them that this treatment exists,” she says. “There are many long-term studies supporting that DBS has positively impacted patients’ quality of life. But 1% of people over the age of 65 will be diagnosed with Parkinson’s disease, and we’re only treating about 70 cases each year – so where are all the others?”
Parkinson’s Europe is sharing this article for information purposes only; it does not represent Parkinson’s Europe’s views and is not an endorsement by Parkinson’s Europe of any particular treatments, therapies or products.


